

Extended-release formulations or sotalol may present later, with deterioration occurring within 24 hours.Ingestion of immediate-release formulations should cause clinical deterioration within ~6-8 hours.Onset of symptoms depends on the medication and formulation:.The high cost and limited availability of glucagon may be the only factors precluding its future clinical acceptance. Glucagon-treated patients should be monitored for side effects of nausea, vomiting, hypokalemia, and hyperglycemia.

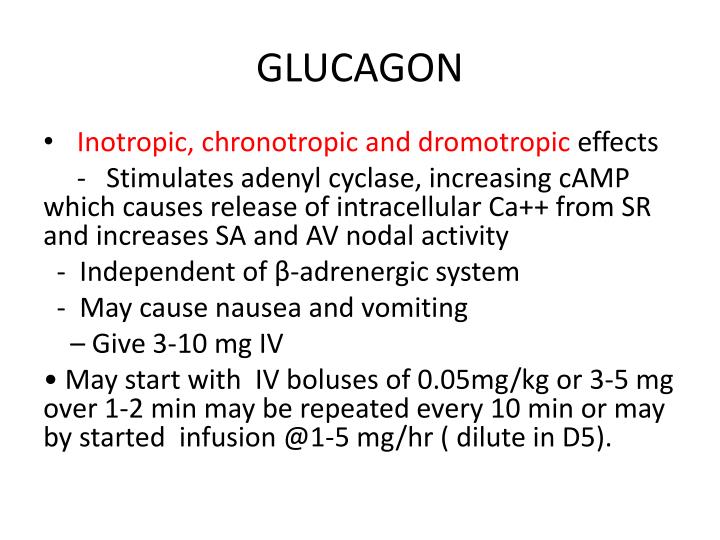
The doses of glucagon required to reverse severe beta-blockade are 50 micrograms/kg iv loading dose, followed by a continuous infusion of 1-15 mg/h, titrated to patient response. Because it may bypass the beta-receptor site, glucagon can be considered as an alternative therapy for profound beta-blocker intoxications. This suggests that glucagon's mechanism of action may bypass the beta-adrenergic receptor site. These effects are unchanged by the presence of beta-receptor blocking drugs. Glucagon increases heart rate and myocardial contractility, and improves atrioventricular conduction. Atropine and isoproterenol have been inconsistent in reversing the bradycardia and hypotension of beta-blocker overdose. Medical complications of beta-blocker overdose include hypotension, bradycardia, heart failure, impaired atrioventricular conduction, bronchospasm and, occasionally, seizures. The effects of glucagon in reversing the cardiovascular depression of profound beta-blockade, including its mechanism of action, onset and duration of action, dosage and administration, cost and availability, and side effects are reviewed. Two cases of severe beta-blocker overdose are presented that were treated successfully with glucagon therapy.


 0 kommentar(er)
0 kommentar(er)
